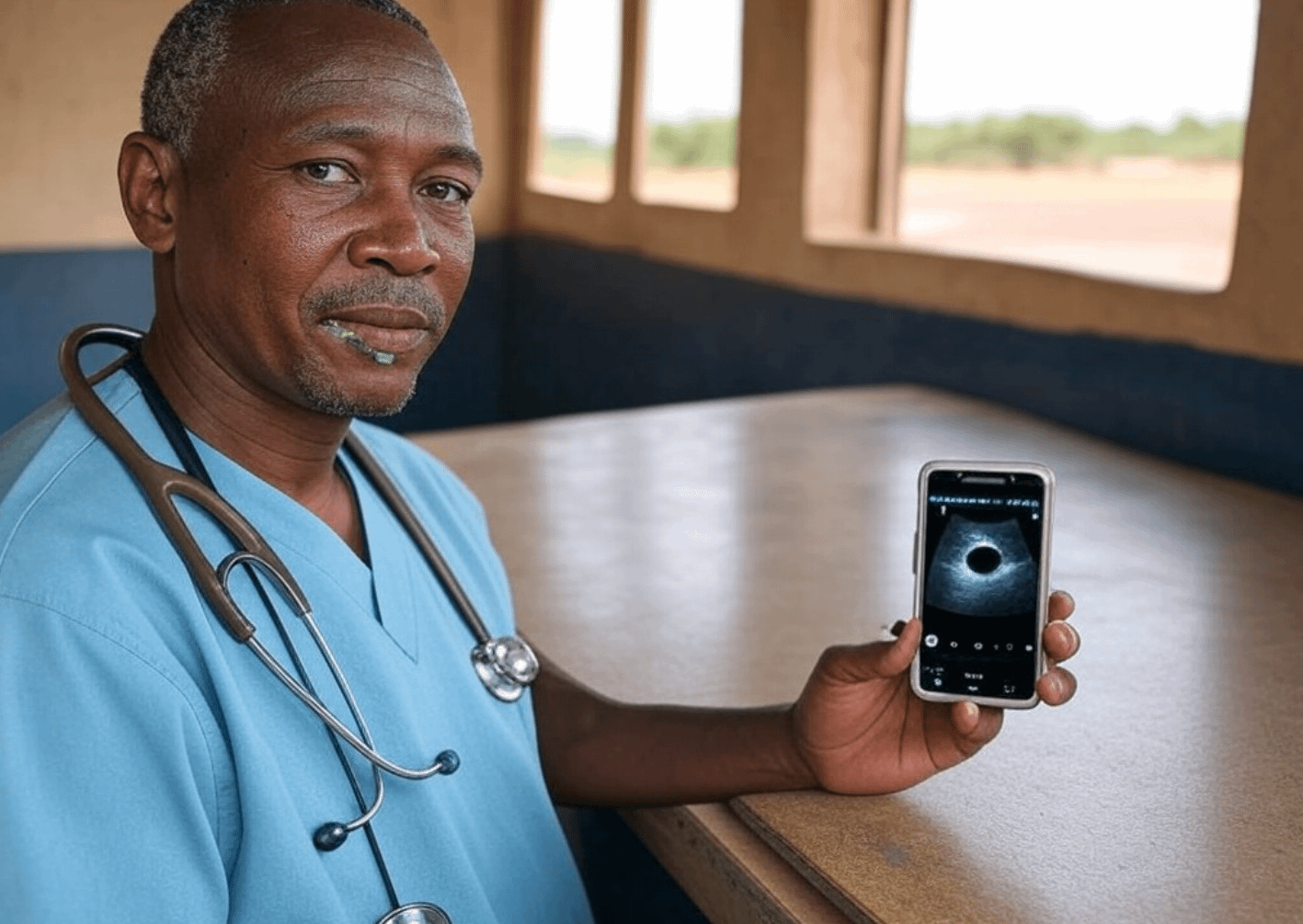
Imagine a world where diagnosing health issues doesn’t require a trip to a distant hospital or the use of expensive, sometimes harmful, technology. With a simple ultrasound device that costs under $500 and an AI system to analyze the images, this vision could become reality, especially in underserved areas of Africa.
The Basic Solution:
- Device: A compact, portable ultrasound scanner, like those from Dr. Sono or similar manufacturers, allows for immediate imaging at the point of care. It’s designed to be user-friendly, with minimal setup required.
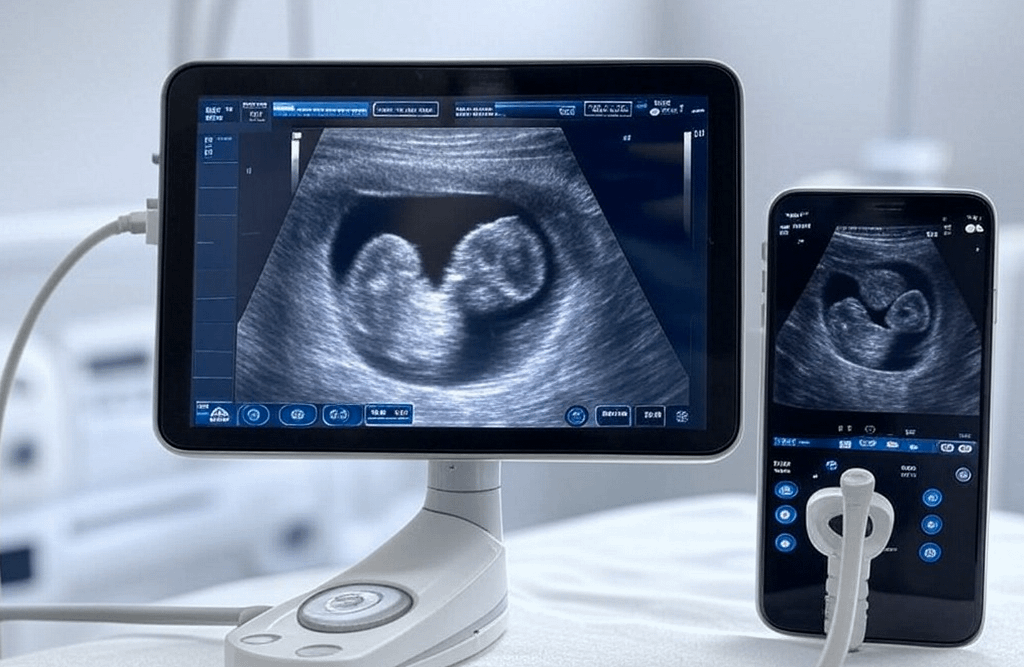
- AI Analysis: Once images are captured, they are processed by AI software, which could run on a connected smartphone or tablet. This AI interprets the scans, offering insights without the need for an on-site expert.
Competing with Traditional Scans:
Ultrasound, when paired with AI, stands as a formidable competitor to other diagnostic imaging methods:
- Cost-Effectiveness: Unlike MRI or CT scans, which require costly machines and maintenance, ultrasound devices are much cheaper to buy and operate.
- No Radiation: Unlike X-rays, ultrasound uses sound waves, making it safe for repeated use, especially beneficial for monitoring conditions over time.
- Portability: You can take these devices to remote locations where large imaging equipment would never go.
- Real-Time Imaging: Offers immediate feedback, unlike MRI or CT which might take time for image processing and interpretation.
List of Conditions Ultrasound Can Diagnose or Monitor:
- Pregnancy: Monitoring fetal health, detecting gestational age, identifying placental position, and checking for anomalies.
- Breast Cancer: Early detection of lumps or abnormalities in breast tissue, especially useful in dense breasts where mammography might fail.
- Cardiac Conditions: Assessing heart function, detecting fluid around the heart, or looking for signs of heart disease.
- Liver and Gallbladder: Identifying stones, tumors, or signs of liver disease like cirrhosis.
- Kidney Disorders: Detecting kidney stones, assessing kidney size, or checking for hydronephrosis.
- Thyroid: Diagnosing nodules or goiter, which can lead to early treatment of thyroid conditions.
- Musculoskeletal: Evaluating joint inflammation, muscle tears, or tendon issues without the need for invasive procedures.
- Emergency Medicine: Quick identification of internal bleeding, appendicitis, or pneumothorax.
- Vascular Health: Checking for blood clots, aneurysms, or assessing blood flow in veins and arteries.
- Pediatrics: Safe imaging for children, from detecting hip dysplasia to evaluating abdominal conditions.
- Prostate: Useful in examining the prostate for signs of cancer or enlargement.
- Lung: Monitoring for pleural effusion or pneumonia, providing an alternative to chest X-rays in resource-limited settings.
- Soft Tissue Injuries: Diagnosing sports injuries like ACL tears or rotator cuff damage.
- Neurological: Assessing for hydrocephalus or any brain abnormalities in infants through cranial ultrasound.
- Ocular Health: Checking for retinal detachment or other eye conditions without the invasiveness of other methods.
Real Numbers, Real Impact:
- Breast Cancer in Africa: According to the World Health Organization, breast cancer is the most common cancer among women in Africa, with an estimated 141,000 new cases in 2020, leading to about 74,000 deaths. The late diagnosis due to lack of screening facilities significantly contributes to these high mortality rates.
- Screening Gaps: In many African countries, there are only a few mammography machines per million women, severely limiting screening capabilities.
- Survival Rates: Five-year survival rates for breast cancer can be as low as 40% in some African regions, compared to over 90% in high-income countries, primarily due to late-stage diagnosis.
Healthcare Workforce in Africa:
- Doctor to Population Ratio: Africa has a significant shortage of healthcare professionals. As per WHO data, the continent averages only about 2.6 doctors per 10,000 people. This stark contrast highlights the challenge in providing adequate medical care. In terms of raw numbers, there are approximately 300,000 doctors for a population that exceeds 1.3 billion, translating to roughly one doctor for every 4,333 people. This ratio is far below the WHO recommendation of 10 doctors per 10,000 people for effective health service coverage.
The Potential Impact:
- Early Detection: Studies suggest that ultrasound combined with AI could increase detection rates by up to 35.7% over mammography alone in dense breasts, which are more common in African populations. Early detection could shift the stage at diagnosis, potentially doubling survival rates if caught early.
- Cost-Effectiveness: With devices priced under $500, coupled with AI software that can be deployed on existing mobile technology, the cost per screening could drop significantly, making regular screening feasible in low-resource settings.
- Reduction in Late-Stage Diagnoses: By enabling earlier intervention, the percentage of women diagnosed with late-stage breast cancer could decrease, directly impacting survival statistics.
- Socioeconomic Impact: Improved health outcomes would reduce the economic burden on families and healthcare systems, potentially saving billions in treatment costs and productivity losses.
By focusing purely on this duo of low-cost ultrasound and AI analysis, we’re looking at a future where millions gain access to diagnostics that were once out of reach, potentially altering health outcomes across the continent despite the current doctor-to-population ratios. It’s about bringing hope and health closer to home, one scan at a time.